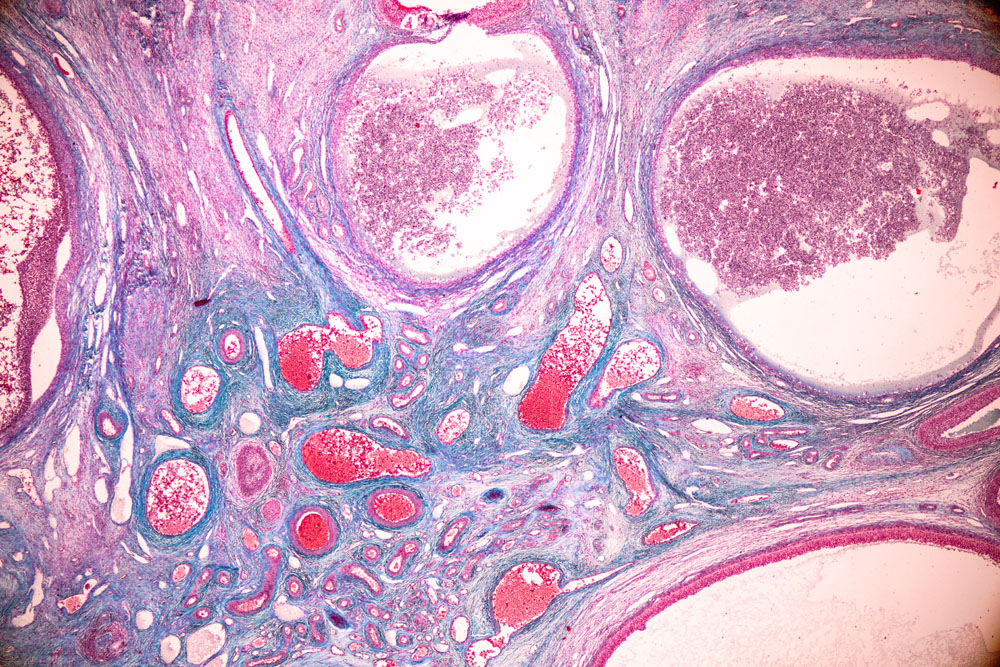
Contrary to what your gynecologist may have told you, having a baby is often not so easy if you were diagnosed with polycystic ovary syndrome, or PCOS for short. To begin with, a large percentage of women in our country manifest with signs and symptoms of PCOS. However, not all cases look the same or have the same severity.
Many women have signs of hyperandrogenism with unusual patterns of hair growth or weight distribution. Acne is common. Harder to see are the changes in glucose metabolism and the irregular or absent menstrual cycles. Read my article Options for Women With Polycystic Ovary Syndrome to gain a better understanding of the complexities of PCOS.
It is still common for gynecologists to recommend to women with PCOS that they use oral contraceptives to establish regular menstrual cycles. One of the arguments is that women with PCOS have a higher risk of endometrial cancer, possibly associated with endometrial hyperplasia due to hormonal imbalances. While hormonal birth control pills can impose a regular rhythm on your irregular or infrequent menstrual cycles, they do not address the underlying condition. Women are usually recommended to stay on oral contraceptives until they wish to conceive. They will then stop these artificial hormone products and take clomiphene, sometimes in combination with metformin, to promote ovulation. This approach works for a small percentage of women but many other women are left out in the cold. They either don’t conceive or lose their pregnancy along the way. Again, this strategy does not address the underlying cause of the fertility challenges experienced by women with PCOS.
PCOS is an endocrine disorder with far-reaching consequences
While it is still somewhat of a mystery what actually causes PCOS, the last several decades of researching this condition have revealed several mechanisms that can be supported with lifestyle medicine, namely nutrition strategies, nutraceuticals and botanicals. PCOS should not be ignored because of the associated long-term health risks and psychosocial challenges women encounter. However, understanding and addressing the hormonal and metabolic imbalances involved in PCOS are crucial in the context of reproduction to increase a woman’s chances of conceiving naturally and carrying a pregnancy to term. Here are some of the latest insights you should know about:
Strategies for women with PCOS
If you have PCOS, you should talk with your naturopathic practitioner about the usefulness of myo-inositol. An important aspect of PCOS and metabolic syndrome that can interfere with fertility is insulin resistance. Inositol is a sugar considered part of the B vitamin family (our bodies do produce inositol, so it’s not technically a vitamin). Women with PCOS appear to be deficient in this substance, which is important for proper glucose metabolism. Fortunately, supplementing myo-inositol is fairly easy, safe and effective. Studies have confirmed that women taking myo-inositol as a supplement for several months experience considerably more regular menstrual cycles and ovulation. It has also been observed to be helpful for women with PCOS undergoing IVF. Myo-inositol may reduce miscarriage and the risk of gestational diabetes. Some women ovulate more consistently by taking a combination of myo-inositol and D-chiro inositol, but the science is not entirely clear whether or not this strategy actually confers an advantage. Discuss dosages and time of administration with your naturopathic practitioner, who can also explain the usefulness of several other nutritional supplements for women with PCOS.
Considering that glucose metabolism and insulin resistance play such an important role in many cases of PCOS, a nutrition strategy tailored to women with PCOS can make a huge difference, not only in connection with your desire to have a baby. I have worked with numerous women, tweaking their dietary approach over the course of several weeks and months, often with impressive results. A Chinese medicine or naturopathic practitioner specializing in PCOS and metabolic syndrome will be a great addition to your team for guidance and feedback. As with many other metabolic and endocrine disorders, a foundational nutrition strategy will allow you to experience improved quality of life and likely a reduced reliance on pharmacological management.
Botanical medicine, East and West
There are also several botanicals that have been used successfully to moderate the symptoms of PCOS and restore regular menstrual cycles. They range from Chinese to Ayurvedic to Western herbs and include such luminaries as Vitex agnus-castus (chaste tree berry). To select appropriate combinations and dosages or forms of administration for these medicinal herbs in order to derive maximum benefit, working with an experienced Chinese medicine or naturopathic practitioner will pay off.
Starting early for best long-term benefits
The energetic imbalances manifesting in women with PCOS can also be addressed with acupuncture. In my experience, they are extremely helpful but should be combined with the intelligent use of nutrition therapy, supplements, and botanical medicine. What you will learn and experience through a series of acupuncture treatments can pay off and serve you well in the long term, so it may be worthwhile investing your time and resources while your you’re trying to conceive. Starting at least 3-6 months before your attempt provides maximum benefit.
© 2025 Christiane Siebert



